YOUR EYE CARE EXPERIENCE

We pride ourselves on the thoroughness of our eye examinations. All of our Optometrist do comprehensive eye tests to ensure you obtain the best outcome for your eye concerns.
To determine your prescription it is done in 3 ways, firstly with our Nidek auto-refractor which gives us a starting, then by using a phoropter, and followed by a free space trial framing of your prescription. We then do extensive tests to examine how your eyes perform binocularly as a team both in the distance and up close. Once we have this information we will then compare it to your old glasses to come up with a new clear and comfortable prescription.
Lastly, we perform a thorough detailed ocular health exam of the anterior (external) eye followed by a pupil dilation to examine the posterior (internal) eye.
- Retinal photography
- Ocular Coherence Tomography
- Humphery Visual field testing
- Corneal Topography
- Optical Biometry and Pachymetry

To understand the benefits of retinal photography, we first have to understand the anatomy of the eye.
The amount of light that enters the eye is controlled by an aperture (much like a camera aperture) called the pupil. The pupil can constrict and dilate according to what distance the focusing object is. Because the pupil constricts and dilates according to light in the surrounding environment (it will constrict in bright light, and dilate in dim environments) it gives a limited view of the back surface of the eye, termed the retina. The retina is a very important structure at the very back of the eyeball that is responsible for absorbing light (that is let in by the pupil) and translating it into electrical impulses to be sent to the brain for image processing. The retina has an important structure, termed the optic disc, that holds the optic nerve and retinal blood vessels, which send information to the brain and supply the ocular structures with appropriate nutrients respectively.
This is why retinal photography is needed – to image the back of the eye and get a much wider, stationary, digital view that helps with analysing ocular health. The retina is prone to many diseases that can be detected even before symptoms are presented. Although retinal photography will not replace the eye examination in itself, it is highly beneficial in helping your optometrist in adding precision.
Retinal photography is especially helpful for an individual if they have the following conditions:
Diabetes – a diabetic’s retina is mostly affected by leaky blood vessels which can potentially cause vision loss and blindness if not appropriately managed.
Age related macular degeneration – where the macular region of the retina (the area where central vision arises) is compromised by drusen deposits. This cases a loss in vision, which can be consequently debilitating.
Glaucoma – where increased pressure on the optic nerve head causes damage, and a consequential loss in peripheral vision.
WHAT HAPPENS IN A RETINAL PHOTOGRAPHY EXAM?
We will first have to dilate your eyes using special drops first. After about 10-20 minutes, your pupil has widened enough for the imaging to take place. At Eyecare Network, we use the Nidek retinal camera to image your retina. At the machine, you will be asked to look at a green light at the centre and to keep your eyes open super wide. The machine will flash and the image is taken. A regular test with retinal photography takes 5 minutes.
BLURRY VISION AFTER DILATION
As the retinal photography test requires eye dilation, these drops will have an impact 4 hours after your examination. Your vision may be blurry and you may be sensitive to sunlight during this time. It is recommended that you bring a pair of sunglasses with you after your examination, and that you have someone to drive you home.

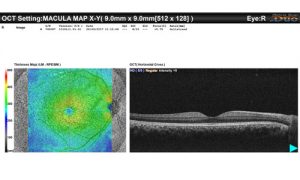
This is like a CT scan of the eye and allows us to see into the deeper layers of the eye
Optical coherence tomography (OCT) is a non-invasive method of imaging the layers of the retina at the back of the eye. The retina has 10 layers, each with their own purpose to help the conversion of light into electrical signals to be sent to the brain. Detecting abnormalities in thickness of the retinal layers is important for diagnosing a variety of retinal conditions such as glaucoma, age-related macular degeneration and diabetic retinopathy. This will also guide treatment for these ocular conditions.
WHAT HAPPENS IN AN OCT EXAM?
To prepare for an OCT examination, your optometrist will dilate your eye to widen the pupil. This creates a larger aperture for the machine to examine and scan the back of the eye. The machine will then use light waves to take cross-section pictures of your retina. It will not touch your eye at all, and the scan takes about 5-10 minutes. As you were dilated before the eye examination, your eyes will remain blurry for about 4 hours after. An OCT examination usually does hand in hand with retinal photography.

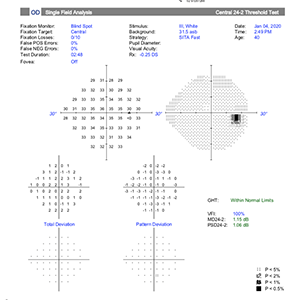
Used to check your peripheral vision for conditions like glaucoma or scotoma induced by a pituitary tumour. We also use this to assess for RMS for commercial and non commercial driving standard using the binocular Estermann test.
A visual field examination is used to diagnose glaucoma, a disease that affects optic nerve head at the back of the eye. In glaucoma, peripheral vision deteriorates progressively and will make its way to central vision. . A visual field test is used to determine the outer extent of one’s visual field – that is, the furthurest they can see whilst keeping their eyes fixated at one location.
WHAT HAPPENS IN A VISUAL FIELD EXAM?
A visual field examination will require the patient to cover one eye at a time using an eye patch. Lenses with the most current prescription are then placed into the machine to ensure the patient has the best corrected vision.The patient then has to fixate on a distant yellow light located within a white bowl. The machine will then spontaneously flash bright white stimuli at peripheral areas of the surrounding bowl. The patient then presses on a button that will indicate whether or not they have seen the flashing light in their periphery. The examination takes about 3-6 minutes each eye.
To make a proper diagnosis of glaucoma, an optometrist may require a patient to sit several rounds of visual field testing. This is to ensure that a reliable and definitive outcome is gathered between tests so that a proper diagnosis can be made. Glaucoma is a progressive condition. Progressive damage to the optic.

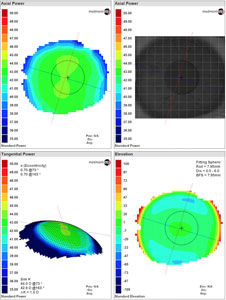
Used to scan the cornea to fit contact lenses as well as diagnose and monitor conditions like keratoconus
Corneal topography is a machine used to examine the front portion of the eye, termed the cornea. The cornea is the most important refractive component of the eye as it is the first medium that light transmits through, before reaching more complex structures like the retina. Corneal topography works by scanning the topography of the cornea, just like in geography, to fit contact lenses. It can also be used to diagnose and monitor conditions like keratoconus. Corneal topography may detect a cornea that deviates from the normal and healthy rounded shape. A cornea that is too flat, steep or uneven is a sign of an underlying condition and may result in vision that is less than perfect.
WHAT HAPPENS IN A CORNEAL TOPOGRAPHY EXAM?
Corneal topography is painless and quick, and does not require dilation. A corneal topographer will have a lighted bowl consisting of concentric rings. Each of these rings are shone onto the cornea and computer software is used to analyse the distortion, or lack of distortion, of these reflected rings. The computer software uses these data points to produce a final topographic map of the front surface of the eye.

Is an ultrasound for the eye which we use to measure the corneal thickness to assess the risk factors for a glaucoma suspect as well as monitoring the Axial length of the eye which is highly useful for myopia control and management
What are ocular biometry and pachymetry?
Ocular biometry is an ultrasound for the eye that takes measurements including axial length (length of the eyeball) and anterior chamber depth (the space between the cornea and iris). Pachymetry refers to the measurement of the central corneal thickness.
Ocular biometry and pachymetry are both highly accurate and non-invasive tests that can be done in just a few seconds.
How we use ocular biometry and pachymetry
At Eyecare Network, we use biometry and pachymetry for myopia control and management, assessing the risk of glaucoma and screening of other eye disorders.
Axial length is important in myopia control and management as the eyeball continuously grows throughout life. As myopia is associated with having a longer eyeball length than normal, it is important to monitor this growth as longer axial lengths (or higher levels of myopia) are associated with higher risks of eye diseases, such as myopic macular degeneration, retinal detachment and glaucoma.
Ocular biometry can also be used to assess the risk of glaucoma by measuring the anterior chamber depth of the eye. Glaucoma usually occurs when the optic nerve at the back of the eye becomes damaged due to the high pressure within the eye. This is often associated with having a shorter anterior chamber depth as this causes the blockage of the eye’s drainage system, which consequently leads to high intraocular pressure.
Central corneal thickness is used in keratoconus screening as the cornea bulges at the centre. This causes the cornea to become thinned in this area and can lead to high levels of astigmatism.
Pachymetry is also useful for screening glaucoma suspects as it allows for further confirmation of the eye’s intraocular pressure.